In late 2014, a BBC News article, “Superbugs to kill more than cancer by 2050,” discussed a UK government review that suggested an additional 10 million people worldwide will die as a result of drug-resistant infections, with an economic impact of $100 trillion. Currently, antibiotic-resistant bugs are implicated in 700,000 deaths each year. Increased awareness about the dangers of antimicrobial resistance has driven increased consumer and government pressure for prudent use of antibiotics, extending beyond human health care to focus on antibiotic administration in animal agriculture.
The link between antibiotic-resistant bacteria and agriculture
The UK study found that drug-resistant E. coli, malaria and tuberculosis will have the biggest impact on the additional deaths by 2050.
E.coli and Salmonella are responsible for a growing level of drug-resistant infections. Both are gram-negative bacteria with a complex cell wall that acts as a barrier to antibiotics. If they do get through, the bacterial cells have a way of “vacuuming” them out. This natural resistance mechanism makes it difficult to find effective drugs.
In the UK, the University of Birmingham is looking at ways to make the bacteria more sensitive to antibiotics. Researchers are investigating the switches that turn off the “vacuum” mechanism these bacteria have, as well molecules, which would have the same effect.
The most resistant organisms are being found in hospitals. The two commonly discussed resistance problems are Methicillin-Resistant Staphylococcus aureus (MRSA) and Extended Spectrum Beta-lactamases (ESBLs). ESBLs are enzymes, which inactivate antibiotics including penicillins and cefalosporins; if the bacterium has the genes for this enzyme, then resistance will occur. Judicious use of antibiotics in these settings could have a large effect on reducing resistant infection rates.
Livestock production has been widely implicated in the spread of ESBLs as these products move through the food chain. For example, studies have shown that 80 to 100 percent of poultry meat tested positive for ESBLs, mainly in E. coli and Salmonella.
Surveillance in the Netherlands shows that most pig and veal calf farms are positive for MRSA. Since the bacterium is transmitted through direct contact, farmers and veterinarians are considered to be potential carriers. Therefore, if they are admitted to a hospital, they are treated in isolation to prevent the spread of MRSA.
Common myths
Some believe antibiotic residues in meat are responsible for increased incidents of resistance; however, antibiotic contamination in carcasses is virtually non-existent. This has been demonstrated by rigorous testing in both the U.S. and Europe.
It is also believe that agriculture contributes to the prevalence of resistant micro-organisms in the environment. This only becomes a human health issue when those bacteria are zoonotic (cause diseases in humans) or are foodborne pathogens, e.g. Salmonella or Campylobacter. These resistant bacteria then spread from the animal population to the human population, where the ability to control the infection is reduced.
Genes capable of transferring resistance from bacteria in livestock to those that cause human infections pose another threat. Figure 1 shows the involvement of humans, livestock and companion animals in the spread of antibiotic resistance, as well as their impact in different habitats.
While the headline grabbing concerns regarding antibiotic resistance relate to human health, these issues can also affect agriculture. As any vet will tell you, treating infections in livestock is becoming more difficult. There will be serious financial implications for the future of producers if disease outbreaks cannot be controlled.
Can antibiotic resistance be reduced?
Although the many factors involved in the increase in antibiotic resistance make it a difficult problem to tackle, there are examples of success.
Ceftiofur, for example, is an antibiotic which isn’t used in broilers, but it had been common practice to use it in grandparent/parent flocks and hatcheries. In 2010, its use was banned in hatcheries in the Netherlands, resulting in a nearly 50 percent reduction in resistance rates in the broiler population.
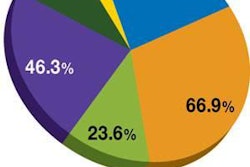
This finding followed a similar trend to that observed when Quebec voluntarily stopped this use of the drug. (Figure 2) After the withdrawal of Ceftiofur in 2005, there was a drastic reduction in the prevalence of resistance in Salmonella Heidelberg in retail chicken and humans, as well as E. coli in retail chicken. This trend continued until mid 2007 when use of the drug was partially reinstated, resulting in an increase in the level of resistant bacteria, although not to pre-2005 levels.
Governments weigh in
Since 2012, the U.S. Food and Drug Administration (FDA) has urged livestock producers to reduce their antibiotic usage. California is looking to stop farmers using preventative antibiotics and the Danish Pig Research Center is aiming to halve the use of the antibiotic tetracycline before the end of 2015.
However, many think legislation is needed in all countries to make a real difference.
“Every time antibiotics are used in any setting, bacteria evolve by developing resistance,” says Steve Solomon, director of the Centers for Disease Control and Prevention (CDC) Office of Antimicrobial Resistance, in a press release. “The more we use antibiotics today, the less likely we are to have effective antibiotics tomorrow.”
The UK government report, mentioned at the start of the article, highlighted the following three areas of investigation:
- How drug use could be changed to reduce the rise of resistance.
- How to boost the development of new drugs.
- The need for coherent international action concerning drug use in humans and animals.
It is only these combined strategies which will work to have a significant effect on the growing problem of antibiotic resistance. Agriculture certainly has a role to play; both farmers and vets should be motivated to use other methods to control and improve the health status of animals – and be responsible for the cautionary and strategic use of antibiotics.
References available upon request.